Causes of the Inflammatory Bowel Disease
The objective of using any medicinal agent is to induce remission of the active disease and maintain remission once the disease has been controlled. The treatment protocol is multifaceted and has to be customized for the patient. Such individualization is dependent on the location and severity of the disease and the presence of complications, if any. The criteria for deciding on the severity of the disease have been laid down by the European Crohn's and Colitis Organisation (ECCO) and the Truelove & Witts Severity Index for Ulcerative Colitis. In addition, monitoring of the response and the presence of side-effects (or tolerability) are also critical to the individualization of the therapy.
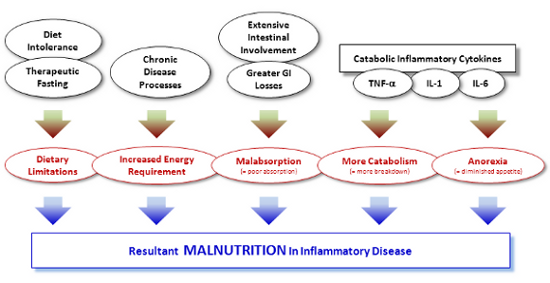
Additionally, focus on nutrition warrants special care not only to correct any nutritional deficiencies that might exist but also to directly impact the anti-inflammatory and recuperative processes.
A. Genetic Factors genetic factor is of greater importance in Crohn's Disease (CD) than in Ulcerative Colitis (UC). The gene involved is known as the NOD2 gene (it is also known as CARD15). This gene is expressed in epithelia cells, Paneth cells, macrophages, dendritic cells and endothelial cells. The gene codes for a protein that is important to recognize and, thus, react to bacterial cell walls, triggering inflammatory process through activation of NF-??.
B. Environmental Factors:
While little is certain, several environmental factors can play a role in the IBD.
- Higher socio-economic status correlates positively with CD. Underexposure to environmental antigens has been proposed as a possible cause.
- Some studies have suggested a correlation with CD with oral contraception.
- Non steroidal anti-rheumatic drugs can exacerbate IBD.
- High amounts of refined sugars and diet deficient in fruits/vegetables have been associated with CD. However, increase dietary fiber content may also aggravate CD.
- Smoking presents a strange case of study. While smoking, predictably, aggravates and precipitates CD, it seems to impart some sort of protection against UC as evidenced by the fact that that UC is primarily associated with non-smokers or ex-smokers. The discrepancy is not yet understood.
- Similar discrepancy has been observed with anxiety/stress. While exacerbations of CD seem to have little correlation with anxiety/stress, UC seems to be more impressionable to anxiety/stress.
- Though there is little compelling evidence, bacterial infections of the intestines have been implicated as possible contributory causes, though the specific bacteria implicated in the two diseases is different. CD has been linked to Mycobacterium paratuberculosis, Pseudomonas spp and Listeria spp. UC, on the other hand, has been linked to Bacillus spp., adhesive Esch. coli and Fusobacterium varium. C. Dietary Factors:
- Breast-feeding has been reported to be protective against IBD in some studies cited by Lucendo and Rezende (2009). Breast-milk affords protection by (a) protection against GI infections, (b) stimulate development of GI mucosa and (c) development of immunological capacity in children (d) postponing exposure to cow-milk-proteins (which are immunogenic). Consumption of cow's milk has been suggested as a causative factor with transmission of Myco. avium paratuberculosis being one possible factor.
- High consumption of sugar and refined carbohydrates has been another suggestive risk factor for IBD.
- Citrous fruits, fruit juices and vegetables could lend a protective influence against IBD.
- Bran consumption is also believed to reduce the risk of developing IBD.
- Associations have been seen between ingestion of partially hydrogenated fats and the risk of developing IBD. Based on study of Eskimo diets, consumption of n-3 polyunsaturated fats (PUFA) is associated with lower incidence of IBD. On the contrary, n-6 PUFA, which are proinflammatory in nature, are implicated in the causation of IBD.
Once again, while definitive and conclusive data is scarce, various nutritional influences have been studied and suggested. Some such suggestions are listed below. At the same time diet gains importance in established cases of IBD not only from the treatment perspective but also from the perspective of correcting the deficiencies that often accompany the disease process due to inadequate intake of food or impaired absorption.
Since a long time, nutritional deficiencies have co-existed with IBD, with the severity being a function of the duration and extent of the disease. Based on different studies, anywhere from 20% to 85% IBD patients suffer from nutritional deficiencies. CD tends to have a more deficiency due to the involvement of the small intestines which are the major site of absorption of nutrients and micronutrients.
Amongst the micronutrients that can run short due to the disease process are: (i) Iron, (ii) Folic Acid, (iii) Vitamin B12, (iv) Iron, (v) zinc, (vi) selenium Data on other micronutrients is lacking and hence it is not possible to comment or conclude about them.
Causes of malnutrition and nutritional deficiencies are diverse and are summarized in the figure below: